Identify novel therapeutic targets for the treatment of Crohn's disease associated fistulas
The focus of this project is the pathogenesis and therapy of fistulas as they represent a frequent and severe complication in Crohn’s disease (CD). Fistulas affect up to 50 % of patients. Therapeutic outcome is often insufficient to achieve fistula closure. Surgical therapy is then necessary. However, fistulae recurrence is very frequent in CD patients.
Using both, clinical materials and in vitro techniques, the group of Prof. Dr. med. M. Scharl has extensively characterized the fistulas in CD patients. We discovered the role of epithelial-to-mesenchymal-transition (EMT) and further defined the mechanisms of extracellular matrix (ECM) remodelling and inflammation in CD-associated fistulae. Also, a novel xenograft model of intestinal fistulas has been characterized in our lab.
Within this project, we will continue to dissect the exact mechanism leading to fistula formation in CD patients and to identify novel therapeutic targets.
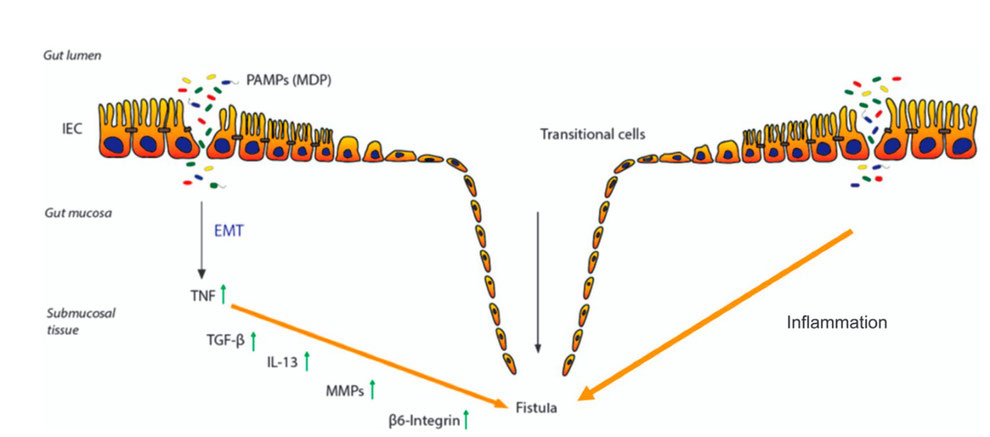
Pathogenesis of Crohn’s disease-associated fistulae.
Due to an epithelial barrier defect several pathogen-associated molecular patterns (PAMPs), like e.g., muramyl-dipeptide (MDP), as well as bacteria are able to enter the gut mucosa. The resulting inflammatory response induces the event of epithelial-to-mesenchymal transition (EMT). First, an increased expression of tumor necrosis factor (TNF) is initiated, resulting in an upregulation of TGF-β production. This triggers a signaling cascade of molecules associated with matrix remodeling, in particular enhanced activity of matrix metalloproteinases (MMPs) and cell invasiveness, such as β6-Integrin. These events favor the transformation of the intestinal epithelial cells (IECs) towards invasive myofibroblast like cells, what finally results in fistula formation.



